Why 2026 Is a Crucial Year for California Health Plans
California has long been a bellwether for healthcare policy in the United States—and 2026 will be no exception. The state’s dual focus on integration and accountability offers a preview of how health plan operations across the country may need to evolve in the years ahead. These shifts affect every California plan type — Medi-Cal, Medi-Medi, Medicare Advantage, local plans, and commercial lines — though the operational pressure points differ.
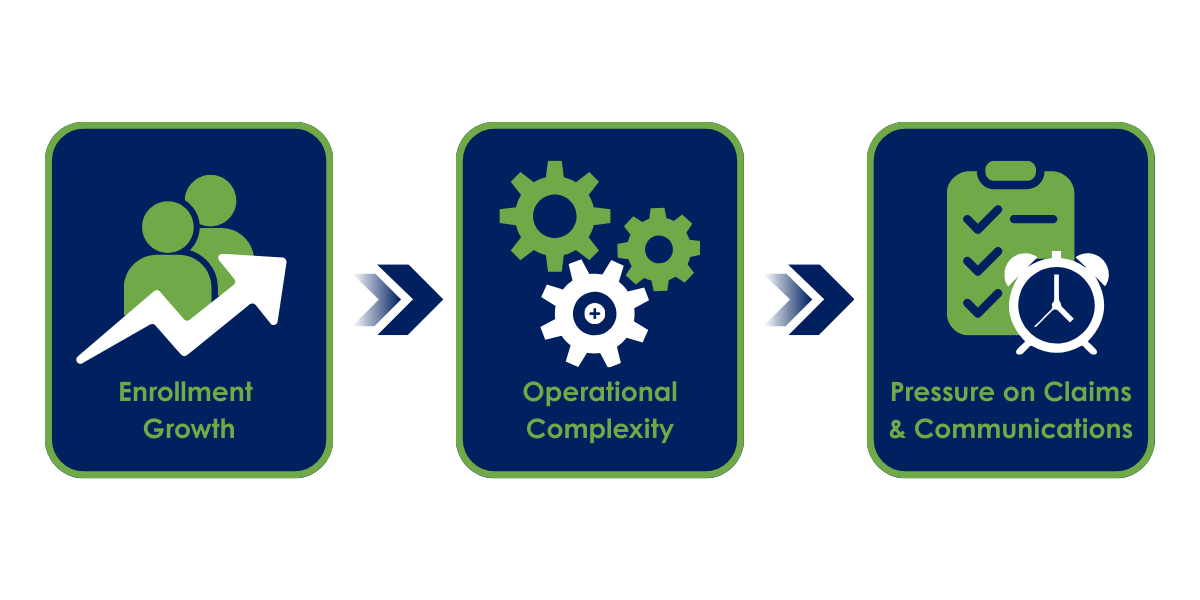
Two developments matter most for day-to-day operations:
Expansion of Medi-Medi (Medicare–Medi-Cal) enrollment across most California counties
A new 30-day clean-claim requirement that applies to all California health plans and insurers
Taken together, these moves are less about incremental compliance and more about speed, clarity, and accountability. They will test how quickly plans can ingest information, adjudicate complex claims, and communicate clearly with members and providers.
Dual-Eligible Growth Meets California’s Operational Reality
Beginning in January 2026, Medi-Medi enrollment will expand across most California counties, ultimately covering 1.7 million Californians—roughly 25% of the state’s Medicare population. The goal is to streamline the experience for dual-eligible members while improving coordination between Medicare and Medi-Cal.
What does claims performance look like when timelines compress?
This infographic highlights the adjudication metrics and operational pressure points that become critical as regulatory timelines tighten. View the Infographic
This expansion increases volume and complexity for Medi-Cal managed care plans with affiliated Medi-Medi plans and local plans with high dual-eligible populations; it also presents two primary challenges:
Greater data integration and cross-program compliance needs
Rising demand for clear, proactive member communication to prevent confusion
Now more than ever, plans must ensure accurate benefit alignment, timely notifications, and well-documented member communications. This requires moving beyond manual coordination to smart, scalable solutions in key areas, including:
Intake & Digital Mailroom
Paper forms, faxed records, appeals, and other member and provider documents still arrive in many formats. When dual-eligible work sits in queues or is keyed manually, it becomes difficult to keep pace with enrollment and benefit changes.
Same-day digitization and intelligent document processing (IDP) help turn mixed paper/PDF/email intake into structured data.
Well-governed intake pipelines make it easier to spot dual-eligible status, coordination of benefits flags, and care-management triggers up front.
Claims Adjudication Capacity
Dual-eligible members often generate more complex claims, with multiple payers, wrap-around benefits, and frequent adjustments.
Flexible, rules-driven workflows and surge-ready capacity help plans keep accuracy and timeliness high, even as claim volumes fluctuate.
Clear worklists and escalation paths reduce the risk that complex claims sit untouched until deadlines are near.
Member and Provider Communications
As member populations diversify and benefits structures become more complex, the burden on communication teams grows:
Member materials must be compliant, multilingual, and clear enough to prevent confusion and complaints.
Provider communication must keep pace with changing payment rules, notification timelines, and documentation standards.
Plans that treat dual-eligible growth as a prompt to modernize operational infrastructure—rather than simply as a compliance exercise—will be better positioned to manage the extra load while improving experience. Together, dual-eligible growth and accelerated claim timelines compress the operating model, raising expectations for speed, visibility, and accountability across all lines of business.
The 30-Day Clean-Claim Requirement: Speed and Accountability for All Plans
The second major change is broader in scope. Effective January 1, 2026, California health plans and insurers either:
Pay complete claims within 30 calendar days, or
Notify providers of contest or denial within the same timeframe
Claims that are not paid or properly contested within the 30-day window may accrue interest, creating direct financial exposure in addition to compliance risk. This requirement applies across the board—including Medi-Cal managed care, Medi-Medi plans, commercial lines, and local health plans. And it creates several immediate operational challenges:
Less time to fix errors. There is less room to chase missing information or correct incomplete claims after the fact.
Heavier reliance on first-pass clean claims. When initial adjudication is wrong or incomplete, the clock is already working against the plan.
Greater scrutiny of timing. Regulators and providers will focus more on whether notices, EOBs, and communications went out within required windows.
Potential surge in inquiries. When visibility is low, provider call volume tends to rise, adding pressure to contact center operations.
Financial penalties add urgency. Missed deadlines can result in interest payments, not just regulatory findings or provider dissatisfaction.
Manual or fragmented workflows struggle under these conditions. When claims miss the 30-day window, interest exposure compounds the cost of rework, making first-pass accuracy and early visibility even more critical. To meet 30-day expectations sustainably, plans need stronger automation and visibility across four areas:
1. Digital Intake – Same- or next-day conversion of paper and unstructured inputs into usable data so claims can move forward quickly.
2. Adjudication Workflows – Configurable routing, worklists, and quality checks that keep claims moving and highlight exceptions early.
3. Provider Communication – Clearly documented notices, EOBs, and status updates with timestamps that support audits and reduce back-and-forth.
4. Provider Support – Real-time access to claim images, notes, and status inside contact center tools so agents can answer questions without delay.
When these pieces work together, compliance becomes more achievable—and plans can use reliability and transparency as differentiators with their provider networks.
How does your claims operation stack up under pressure?
This quick, five-part self-assessment helps California health plans benchmark claims throughput, accuracy, audit readiness, and identify hidden risks. Get the Claims Assessment
What Different California Plan Types Should Take Away
Although Medi-Cal and Medi-Medi are in the spotlight, the implications extend across plan types:
Medi-Cal managed care plans must coordinate dual-eligible integration, member communications, and claims timelines—all under budget pressure.
Local health plans and county-based plans need scalable ways to handle variable volumes tied to local demographics and delegations.
Commercial and Medicare Advantage plans operating in California must adapt to the same 30-day expectations and may see similar rules appear in other states over time.
Across all these segments, a few themes are consistent:
Manual, paper-heavy processes make it extremely difficult to meet tighter timelines.
Disconnected intake, claims, member communications, and contact center operations create blind spots that can lead to noncompliance.
Investments in automation, structured data, and governed workflows pay off quickly when regulatory complexity and volumes rise simultaneously.
What the Rest of the U.S. Needs to Watch and Learn From
California’s healthcare policies historically set the tone for federal- and state-level reforms. These mandates align with broader national trends — Medicaid modernization, dual-eligible integration pilots, and rising expectations for multilingual, audit-ready communication. They offer an early preview of how integration and accountability mandates may evolve across the U.S.
Health plans outside California can use these developments as an early signal of what may be coming next:
Digital transformation is no longer optional: Manual workflows are inherently incompatible with accelerated timelines, audit demands, and multilingual member communication.
Member communication is now a compliance function: Accuracy, timing, and documentation are now as critical as engagement.
Future-proofing requires scalable automation: Building now is faster—and cheaper—than rushing post-mandate.
Preparing for What’s Next: Practical Steps for Health Plan Leaders
Ultimately, these changes signal a shift toward a more modern, accountable operating model — and plans that build readiness now will be in the strongest position. Whether you operate solely in California or across multiple states, the takeaway is the same: expectations are rising, and readiness will matter more than ever. Pragmatically, that means:
1. Modernize intake. Move from paper/fax/email queues to governed digital mailroom pipelines that capture, classify, and route work on the day it arrives.
2. Tighten claims workflows. Ensure complex claims, dual-eligible cases, and edge scenarios are visible early, with clear owners and SLAs.
3. Elevate member communications. Treat ANOCs, EOCs, notices, and outreach as a compliance function as well as an engagement tool—especially for dual-eligible and vulnerable populations.
4. Integrate provider support. Give frontline teams the tools and information they need to answer questions about claims and coverage quickly and accurately.
California’s 2026 mandates aren’t just policy changes— they are signals about where expectations for timeliness, coordination, and transparency are headed. Health plans that invest now in automated, connected, compliant, and member-centric operations will be best positioned to lead.