Realize Optimal Benefits Coordination and Payment Accuracy With Superior MSP and COB Solutions
Streamline compliance, optimize recoveries, and reduce administrative burden.
Optimize Your Revenue Recovery Potential
Healthcare is challenging enough — as are the nuances of Medicare. Adding secondary payers into the mix adds more complexity for health plans that are already wrangling with evolving regulatory and compliance measures, time-sensitive mandates, and staffing and technology challenges. Until now.
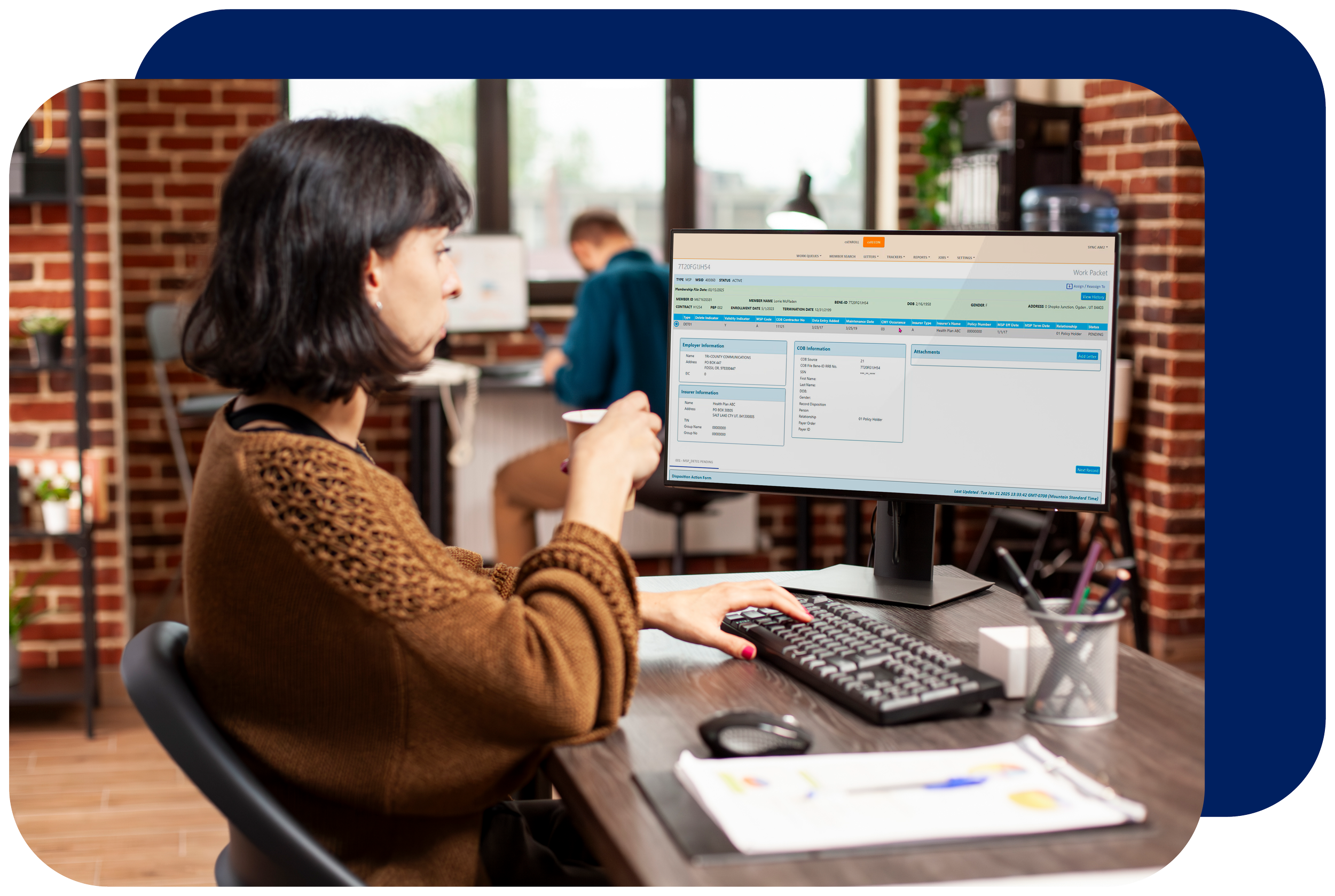
Real-time data synchronization for Medicare Secondary Payer (MSP) by Imagenet—powered by CodySoft®—ensures your plan makes required payments only when it needs to make them, reducing Medicare expenditures and complexities.
Core Capabilities:
Identification and validation of capitation recovery opportunities
De-duplication, record grouping, and tracking of electronic correspondence
Automatic reconciliation of primacy flags within claims payment systems

Empowering Healthcare Payers in Multiple Ways:
Optimal Data Management
Automated & Improved Reconciliation
Ensured Payment Accuracy
Reduced Administrative Burden
Make Real-Time Benefits
Reconciliation Easy
Coordination of Benefits (COB) rules determine how multiple health plans pay insurance claims for one shared member. But it often feels like payers’ "solutions" work against them. That’s where Imagenet’s Coordination of Benefits (COB) Module—powered by CodySoft®—comes in. Working independently, or seamlessly in tandem with our MSP module, our COB solution expertly manages CMS Part D coordination of benefits files.
Core Capabilities:
Identification of new enrollees and annual records with customizable business rules
Automatic and timely updates to downstream claim systems
Proactive identification of overlaps and gaps

Your Revenue Recovery Potential
$700K
In premium recovery from CMS for a Medicare Advantage Organization (MAO) with approximately 32,000 members
$500K
Recovered for a small MAO with approximately 5,000 members
$400K+
Recovered for an MAO with approximately 15,000 members


See What Our Real-Time Benefits Reconciliation & Payment Accuracy Solutions Can Do for You